Apheresis: what you need to know

Therapeutic apheresis is the withdrawal of whole blood from the body, separation of one or more components, and return by transfusion of remaining blood to the donor. Common components that are removed include immunoglobulins, immune complexes, lipoproteins, leucocytes, platelets, and abnormal red cells like sickle cells.
The American Society for Apheresis guideline outlines the effectiveness of apheresis in various disorders (Padmanabhan et al., 2019). The categories, definitions, and common examples are as below. The lower the category number, the greater the evidence for benefit.
Category 1: apheresis accepted as first-line therapy
- haematological: thrombotic thrombocytopenic purpura (TTP), Waldenström macroglobulinemia with symptomatic hyperviscosity or as prophylaxis before rituximab (consider when IgM >40 g/L) (Pratt et al., 2022)
- vasculitides: anti-glomerular basement membrane (GBM) disease complicated by dialysis-dependent renal failure or diffuse alveolar haemorrhage (DAH), ANCA-associated vasculitis complicated by severe rapidly progressive glomerulonephritis or DAH
- neurological: myasthenia gravis, acute and chronic inflammatory demyelinating polyradiculoneuropathy
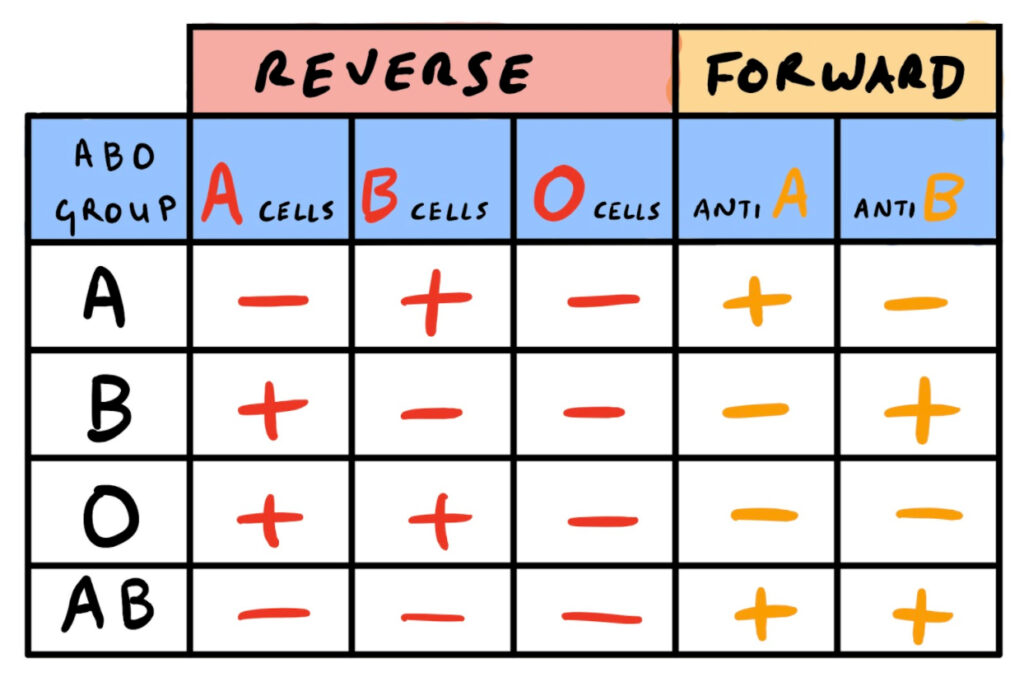
- transplant-related: ABO-incompatible living donor renal transplantation, ABO-compatible renal transplant complicated by antibody-mediated rejection
Category 2: apheresis accepted as second-line therapy
- severe acute chest syndrome in sickle cell disease, steroid-refractory acute disseminated encephalomyelitis, severe/symptomatic cryoglobulinemia
Category 3: optimum role of apheresis not established
- hemophagocytic lymphocytosis, pancreatitis related to hypertriglyceridemia
Category 4: apheresis likely ineffective or harmful
- idiopathic polyarteritis nodosa, gemcitabine/quinine associated thrombotic microangiopathy
The British Society for Haematology guideline outlines the indications, technical aspects, complications, and quality management of apheresis (Howell et al., 2015). Albumin (4.5 or 5%) is the most common replacement fluid due to significantly less adverse reactions compared to plasma. An important exception is TTP where solvent/detergent fresh frozen plasma (FFP) should be used to replace ADAMTS13. FFP should also be considered in high-bleeding risk settings due to the risk of dilutional coagulopathy with albumin, for example, anti-GBM disease complicated by DAH.
In general, it is optimal to exchange 100-150% of the patient’s plasma volume per procedure. Adequate vascular access is achieved by using large-gauge peripheral cannulas or central venous catheters that are also dual-lumen, short and rigid-bodied. The frequency and number of exchanges varies, but a common regimen is five exchanges at 100% plasma volume at daily or alternate-daily intervals. For example, in TTP apheresis should be initiated within 4 hours or presentation and continued daily until platelet count is normal for 3 consecutive days. Plasma volume exchange per session is 150% and reduced to 100% when there’s response.
Complications of apheresis
- vascular-access related: thrombosis, infection, bleeding, air embolus, pneumothorax, arrhythmia
- anticoagulant-related: citrate-related hypocalcaemia and metabolic alkalosis, over-anticoagulation, heparin-induced thrombocytopenia
- blood product-related: transfusion reactions (e.g., anaphylaxis), infection
- albumin-related: dilutional coagulopathy and hypofibrinogenemia, removal of albumin-bound medications
- other: vasovagal reaction, hypovolemia, bradykinin-induced histamine release during lipid apheresis, recirculation
Of note, citrate is present in FFP and often used as an anticoagulant for apheresis. Patients with renal and hepatic impairment are at risk of citrate-induced hypocalcaemia and prophylactic calcium supplements should be considered when receiving citrate anticoagulation. Angiotensin-converting-enzyme inhibitors should be withheld 24-72 hours prior to apheresis as they increase the risk of vasovagal symptoms.
Other important considerations related to the delivery of an apheresis service include identifying a lead clinician, documentation, accreditation, facilities, equipment, staffing, training, and quality management including regular audits.

Author
Dr Jun Yen Ng
Haematology registrar at Canberra Hospital, Australia
Twitter handle: @JN67698874
Want to learn more about haematology?
See our available courses! Our exclusive courses make learning easy.
Accredited by the Royal College of Pathologists.
References
- Howell, C., et al. (2015). Guideline on the clinical use of apheresis procedures for the treatment of patients and collection of cellular therapy products. British Committee for Standards in Haematology. Transfusion Medicine (Oxford, England), 25(2), 57–78. https://doi.org/10.1111/tme.12205
- Padmanabhan, A., et al. (2019). Guidelines on the Use of Therapeutic Apheresis in Clinical Practice – Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue. Journal of Clinical Apheresis, 34(3), 171–354. https://doi.org/10.1002/jca.21705
- Pratt, G., et al. (2022). Guidelines on the diagnosis and management of Waldenström macroglobulinaemia-A British Society for Haematology guideline. British Journal of Haematology. https://doi.org/10.1111/bjh.18036
- Fridey, J., & Kaplan, A. (2022). Therapeutic apheresis (plasma exchange or cytapheresis): Indications and technology. UpToDate. Retrieved February 23, 2022 from https://www.uptodate.com/contents/therapeutic-apheresis-plasma-exchange-or-cytapheresis-indications-and-technology
- Kaplan, A., & Fridey, J. (2022). Therapeutic apheresis (plasma exchange or cytapheresis):
- Complications. UpToDate. Retrieved February 23, 2022 from https://www.uptodate.com/contents/therapeutic-apheresis-plasma-exchange-or-cytapheresis-complications