Case Study – Diagnosis of COVID-19 Vaccine Associated Thrombosis and Thrombocytopenia (VATTS)
Case Study – Diagnosis of Vaccine Associated Thrombosis and Thrombocytopenia (VATTS)
* Use of D-dimer for the investigation of suspected case of venous thromboembolism.*
A 39 year old male presented to A&E with shortness of breath, the patient had been feeling lethargic, generally unwell and short of breath for several weeks since having his AstraZeneca COVID 19 vaccine but was now short of breath when at rest and unable to walk upstairs. The patient had a dry cough for two weeks, new pleuritic chest pain lasting three days, which was very severe and a had a hot, swollen, tender left leg around two weeks prior to his admission which had now settled. His SpO2 levels were now very low.
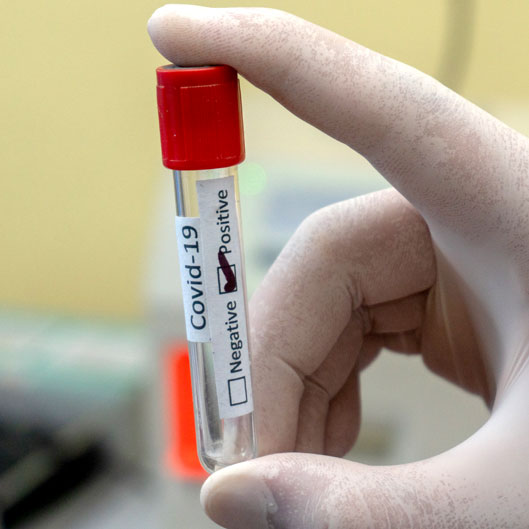
A range of blood tests were requested along with an urgent CT scan, the full blood count results were notably abnormal and the patient was admitted to the Intensive Care Unit.
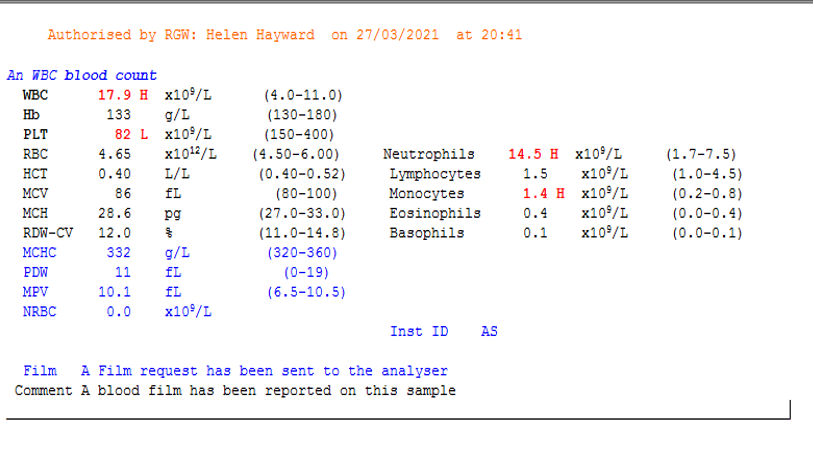 Image 1 – Screenshot of patient’s initial FBC results.
Image 1 – Screenshot of patient’s initial FBC results.
The results show a moderate thrombocytopenia which is unexplained at this point, the sample is checked macroscopically for any clots and a blood film is made and checked for any evidence of platelet clumping which may explain the low platelet count, nothing is detected in the blood film and it is suggested that a repeat full blood count is taken to confirm the thrombocytopenia.
The repeat full blood count shows the platelet count dropping further from 82 x109/L to 55 x109/L in the space of a few hours. At this point the patient is under the care of the intensive care consultant and consultant haematologist, a further repeat full blood count is sent along with a coagulation screen request. The consultant haematologist requests that a blood film is made on this sample and checked for evidence of fragments, this is requested to rule out thrombotic microangiopathy, haemolysis or infection as the cause of the thrombocytopenia. No fragments or platelet clumps are detected in the film indicating a true thrombocytopenia.
A third repeat full blood count is requested on a citrate sample to eliminate the possibility of EDTA dependant platelet agglutination, the full blood count results on this sample are identical to the previous EDTA sample so this cause is eliminated.
The consultant haematologist suggests running a D-dimer level on the citrate sample that was sent, the D-dimer result is >20,000 which is hugely abnormal. A D-dimer level is typically used as a negative predictive indicator for a VTE, a low D-dimer level would indicate that the presence of a clot is very unlikely. In this case the very high level would suggest that a thrombosis of some form has occurred and the patient requires a CT scan to detect the location. A very high D-dimer is uniquely associated with very serious illness, it is primarily an indicator of VTE but can also be associated with malignancy, sepsis and COVID 19 as a transient inflammatory marker. A very high D-dimer must always be investigated.
The urgent CT scan shows a large volume pulmonary emboli, the magnitude of this D dimer result is indicative of the large VTE that the patient has suffered. D dimer is a breakdown product of fibrinolysis and the level is directly proportional to the amount of breakdown that has occurred of cross-linked fibrinogen in the body, the more D-dimer present the larger the thrombosis that has been broken down.
At this point VATTS is suspected.
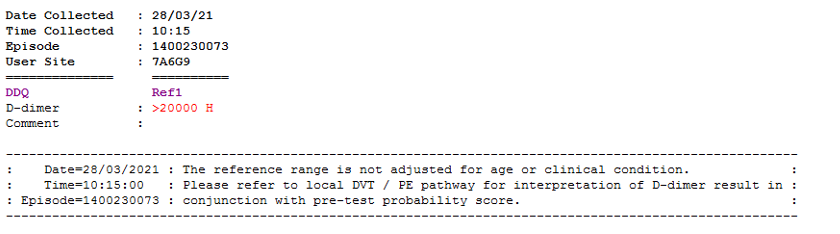 Image 2 – Screenshot of the patients D-dimer screen result, this result is markedly high and fits the criteria for VATTS.
Image 2 – Screenshot of the patients D-dimer screen result, this result is markedly high and fits the criteria for VATTS.
A coagulation screen was also performed and initially shows a high fibrinogen but this drops to the lower end of normal as the patient deteriorates, this could be due to inflammation or because of the massive thromboembolism.
 Image 3 – Overview of the patient’s coagulation screen results.
Image 3 – Overview of the patient’s coagulation screen results.
Vaccine associated thrombosis and thrombocytopenia or VATTS has been detected in a small number of patients throughout the UK within 28 days after administration of the AstraZeneca Vaccine for COVID 19. At present there is no clear guidance on risk factors that may cause this rare syndrome and it has affected patients of all ages and genders.
Typical laboratory findings include a platelet count of <150 x109/L, very raised D dimer levels, above the expected level for VTE, and a low fibrinogen. It is known that VATTS has similarities to heparin induced thrombocytopenia or HIT and the patient should be tested for autoantibodies to platelet factor 4. (1) PF4 IgG autoantibodies are produced and bind to heparin molecules, these antibodies induce platelet activation via the FcγIIa platelet receptors. It is the activation of the platelets that causes the unexplained thrombocytopenia. A similar mechanism is seen in VATTS but the antibody response is activated by the vaccine rather than heparin, therefore a HIT assay should be performed but in the absence of heparin. This will still detect the presence of PF4 autoantibodies as the HIT assay detects the IgG antibodies using an ELISA technique, and is reported as a positive or negative result. (2) Excellent knowledge & understanding of this unique case & HIT assay properties NP 09/04/2021
A sample for a HIT screen is sent urgently to the University Hospital of Wales to their special coagulation department, the assay is performed using their ELISA technique and autoantibodies to platelet factor 4 are confirmed in the sample, the PF4 autoantibodies and the activation of platelets promote thrombosis which is why they are urgently tested so the patient can be treated. Excellent example of urgent clinical & Laboratory action. NP 9.4.21
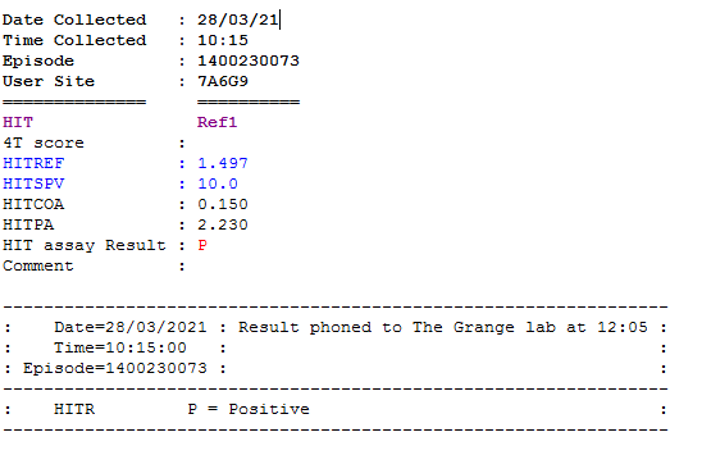 Image 4 – HIT assay result from UHW.
Image 4 – HIT assay result from UHW.
Upon confirmation of the VATTS diagnosis the patient’s heparin infusion is stopped and switched to argotraban, a different anticoagulant, to limit the effect of heparin induced thrombocytopenia. The patient can be switched to a DOAC once they are stabilised, all heparin should be avoided as it is unknown if heparin worsens the condition.
Recommended treatment for VATTS is to give intravenous immunoglobulin to help balance the bleeding and thrombotic risk by slowing the autoimmune response and therefore slowing the rate of platelet activation and destruction. Platelet transfusions should be avoided as it is likely the platelets will just become activated by the PF4 autoantibody complex and will ultimately promote more thrombosis. Steroids and plasma exchange can also be considered to reduce the level of autoantibodies in the bloodstream that are activating the platelets, these can be used until the platelets return to a safe level. (3)
We can see here when the patient was admitted a moderate thrombocytopenia was detected, this has since returned to normal after treatment.
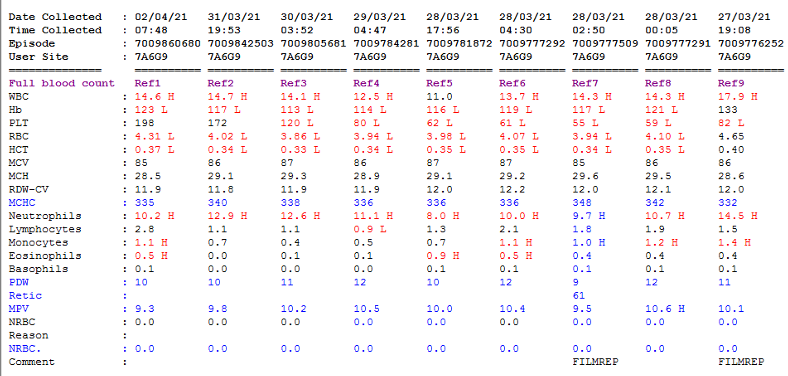 Image 5 – An overview of the patient’s FBC results.
Image 5 – An overview of the patient’s FBC results.
The patient remains on steroid treatment and oral anticoagulant, these will be gradually weaned off and the patient’s reaction will be assessed. This patient has had a rare, life threatening reaction to the COVID 19 vaccine and it is yet unknown if he may relapse. Further samples are sent to Colindale laboratory at Public Health England to be included in a genomics study and for COVID antibody testing, complications of the COVID vaccine are also reported to the MHRA.
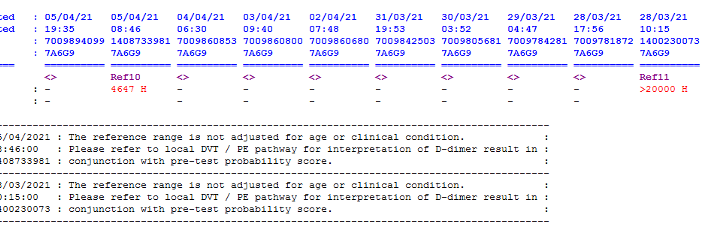 Image 6 – Overview of the patient’s D dimer screen.
Image 6 – Overview of the patient’s D dimer screen.
The patient’s D dimer result is improving after treatment with IVIg, steroids and anticoagulant, in this case it is difficult to assess whether the D dimer is still raised as an indicator of clot breakdown due to the VTE or if the level remains high secondary to the hyper inflammatory state that the patient is in. Either way a clear extended thromboprophylaxis plan should be put in place for the patient to avoid thrombotic relapse.
VATTS Checklist
- Has had a COVID 19 vaccine in the last 28 days
- New onset thrombocytopenia <150×109/L
- Blood film confirms true thrombocytopenia
- Coagulation screen shows a low fibrinogen
- D-dimer result is >4000
- HIT screen gives a positive result
- Thrombocytopenia must be present with thrombosis
References
- Andreas Greinacher, Thomas Thiele, Theodore E. Warkentin, Karin Weisser, Paul Kyrle, Sabine Eichinger. Accessed at A Prothrombotic Thrombocytopenic Disorder Resembling Heparin-Induced Thrombocytopenia Following Coronavirus-19 Vaccination | Research Square. On 07.04.21
- Theodore E. Warkentin MD, FACP, FRCPC, FRCP(Edin), in Consultative Hemostasis and Thrombosis (Fourth Edition), 2019. Accessed at Heparin-Induced Thrombocytopenia – ScienceDirect. On 07.04.21
- Immune thrombocytopenic purpura (ITP). Accessed at pdf (ouh.nhs.uk). On 07.04.21




